History of the Surgery Technique
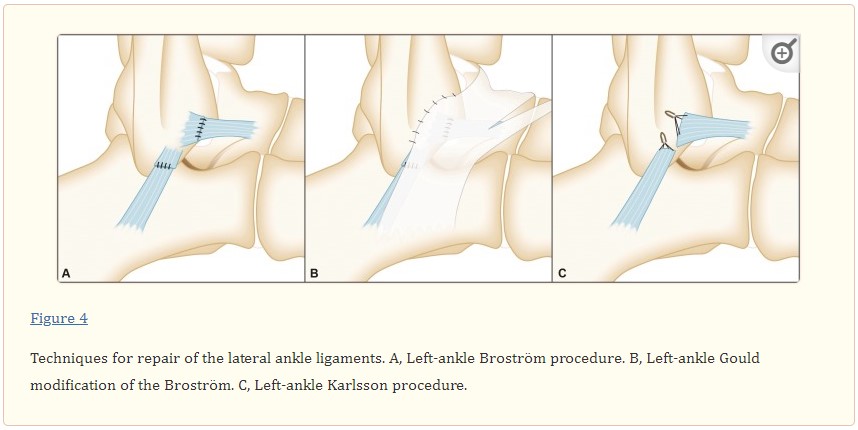
History of the Surgery: The Brostrom Technique initially described in 1966 is a surgical technique for reconstructing the lateral ankle ligaments including the anterior talofibular ligament (ATFL) and calcaneofibular ligament (CFL). Both the ATFL and CFL are primary passive stabilizers of the ankle that resist inversion and plantarflexion. After these ligaments are initially injured, the weakening of the ligament combined with the increased forces that move through the ankle complex often result in an increased reinjury rate. Over time this loss of stability predisposes the ankle joint to increased stress/strain and potential injury of surrounding structures. The purpose of the Brostrom technique and its subsequent modifications is to restore stability in the unstable ankle and improve dynamic function in the ankle complex.
Camacho LD, Roward ZT, Deng Y, Latt LD. Surgical Management of Lateral Ankle Instability in Athletes. J Athl Train. 2019 Jun;54(6):639-649. doi: 10.4085/1062-6050-348-18. PMID: 31238016; PMCID: PMC6602388.
Injury Background: Playing baseball, basketball, running track and being very active in sports since I was in elementary school, I never really had any significant injury until graduate school. Funny enough, it was playing flag football in an intramural game when I initially injured my ankle. I caught the ball, pivoted right with my body to avoid a defender in front of me while my ankle was planted going left. I got tripped up with the defender going into my side causing me to fall with my ankle inverting plantarflexing and going left while my body went right. I heard a pop and saw it start to swell up. I hobbled over to the sideline and that was it. I was in crutches and a hard brace for 2 weeks, but I could tell it wasn’t really the same. Ever since then, I would have a low level sprain on average about 1-2x/yr, but was able to rehab myself out of it.
Fast forward to my most recent injury resulting in this surgery, I was playing tennis in a club league when I was backing up at an angle trying to get the ball. My foot gripped the hard-court as my body went back causing me to trip and roll my ankle again with my foot going right under me. Unlike the other times, I wasn’t able to rehab this over several months. I would get baseline ankle soreness that would last for hours. It would feel sharp whenever I pivoted/twisted to play tennis and , worse without an ankle brace. Moving the wrong way without my brace would result in significant instantaneous pain with a background lingering. Because of these, I would change my activity level and how I moved to avoid painful movements. Unlike the previous times where I was able to rehab and recover, this time I couldn’t get over the hump of avoiding painful movements and background pain with activities I wanted to pursue.
After consulting with the ortho surgeon, I opted to proceed with the Modified Brostrom with internal brace surgery.
Pre-hab Before Surgery:
In the realm of physical therapy and ortho surgery rehab, there are factors that can improve post-operative success pre-operatively that are within your ability to control:
- Pre-conditioning the area – Surgery inherently traumatizes the area because it is going in invasively to fix an issue. The tissues are traumatized along the surgical site and wherever that blade cuts or drill penetrates is an area of tissue trauma. To improve success, the area of the surgery and around the surgery should be pre-conditioned and strengthened to resist the surgical trauma and rebound quicker during post-surgical recovery.
- Strengthen the chain – Compensatory strategies are inevitable with every lower extremity surgery. Walking on one leg is not a normal movement pattern for someone who is used to walking on two legs. In rehab, when one structure is not working, the load, stress and demand has to go somewhere. In the movement chain, this results in that force getting pushed into the structures above, below it and on the other side in compensation. Over time, that increased demand on structures not used to the stress may result in them overloading, breaking down or failing. Strengthening and reinforcing these segments above, below and on the other side become important for resisting the overload and stress of post-operative compensation.
Knowing that surgery was on the horizon, I went to work strengthening, promoting dynamic stabilization, optimizing balance and improving endurance in my core and of my foot and ankle, knee and hip on both sides over 2 months. I also went about acquiring equipment that would be helpful to improve healing, pain control., mobility and safety.

Operation Day and Post-op Day 0-1:
Going into the surgical center at VCU Health in Short Pump, everything was fairly relaxed. A rotating group of nurses and medical doctors came through to verify identification and agreement to what was going to be done and where. The anesthesiology team decided to give me a nerve block to help ease the pain and improve comfort for the first day. After it was administered my leg became gradually warmer, tingly and finally dead numb almost like if you cut off circulation to an area or if you slept the wrong way. It personally felt that my leg was not apart of my body when I could move my knee, but couldn’t move or feel my ankle though I was able to see it and internally know it was attached to me. Something surreal.
Finally it came time to bring me back to the OR. I remember the OR team being awesome; getting wheeled into the room to the sound of pump up the jam and some 80s power ballads with the team being friendly and welcoming me while I was throwing some light jabs and receiving them, completely got me into a relaxed mood. I wasn’t under anesthesia at this point and slid over to the op table where the procedure was going to take place. A nasal mask was used to provide oxygen while my IV line was setup. The nurse who administered the anesthesia kept talking to me and finally said “it’s time, you’re going to start to relax”. I remember feeling relaxed already and understanding that I’m about to have surgery. I closed my eyes and I remember seeing initially black, then I could see the black turn to an orange, red and then white which was trippy since my eyes were closed. I remember verbally describing what I was seeing, but all I could hear were faint laughs.
When I came to, I was sitting up in the bed in the recovery room. If you’ve never been through anesthesia for hours, the confusion of the loss of time and events over that period is indescribable. I tried to recall what happened, but I couldn’t. I remember looking down at my foot to see if they actually did the surgery and saw that my foot had soft-cast on it. I still couldn’t feel anything or move anything below my knee because of the nerve block. Again, very surreal thinking that there should be some kind of sensation after having surgery, but then not experiencing it kinda shocked my mind. The nurse who was watching over me kept talking to me asking questions that I no longer remember after I came to. I can remember that she was laughing at a few things I said. Maybe I was making a joke or talking gibberish. Gradually I became more alert and I realized where I was, what happened and that the first part was over.

The old adage of you never really know what it’s like until you experience it yourself is true. Understanding that I only had one good leg and I couldn’t put weight on my R foot posed some immense initial challenges. Getting up the 3 steps to get into my house using crutches, one foot and a hand on the rail was difficult and I could picture myself falling if I was just a little off balance. Once inside, getting my knee scooter and moving quickly on because I was overconfident resulted in a fall to the ground. I remember moving through my house on the scooter, turning but keeping a lot of my weight on my R knee which resulted in my weight shifting to the side and subsequently sliding off the scooter to the ground. In order to protect my surgical foot, in the last moment before I hit the ground, I lifted my entire R leg up to avoid impacting the ground. Thankfully I didn’t injury anything, but it was then that I realized how if I don’t work on slowly getting used to my environmental conditions and my mobility tools, I was in for a rude awakening. Being a PT, I needed to separate my external understanding from my actual experience. Retraining myself on how to move around the house, how to use the bathroom and how to navigate taking care of daily activities was and is a learning experience. It’s the start of a journey towards recovery.

